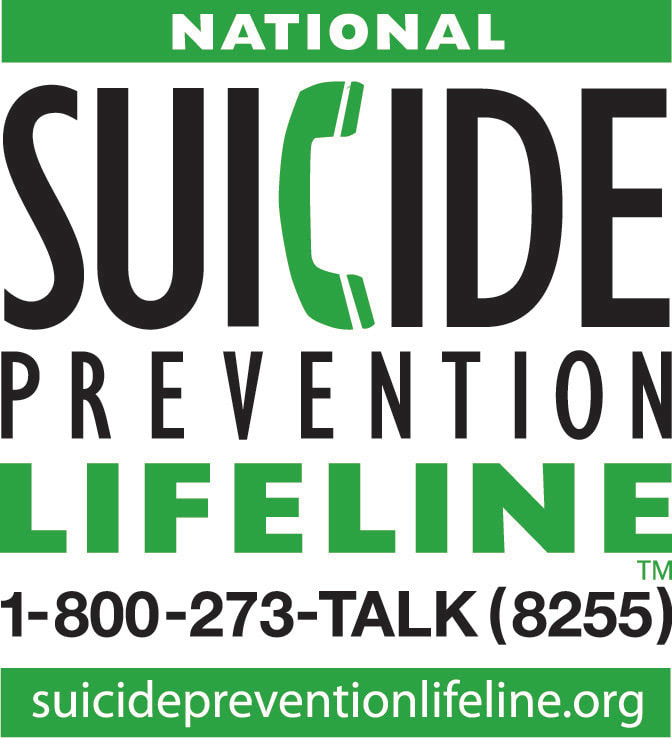
| My blood is boiling! I am a mental health counselor because I WANT to help people. I understand that life can be difficult and therefore, quality, genuine support is necessary. However, it is not always accessible or affordable to the individuals who need help the most. I choose to participate with health insurance companies as an in-network provider as part of my advocacy for helping people. Many therapists (and I mean, the majority of them!) in the Atlanta area do not accept insurance for mental health services. This means a potential client has to decide if they can afford to pay the full price of counseling in order to receive effective treatment. Some clients are blessed financially to be able to afford this luxury. Others, are not – but these people deserve to receive quality therapeutic services as well! |
- Time: It can take an hour or more (per client) to access a representative to discuss benefits, claims, preauthorization. This is BEFORE seeing a client for the initial session.
- Payment Delay: It takes 7-14 days to receive payment after a claim is submitted.

- Claim Issues: If a claim is denied or other issues arise with payment, the provider must re-contact the insurance company to advocate (fight) for a resolution. This can require several calls and hours of UNPAID time. ** This is why my blood is boiling today! Yes, Anthem BlueCross BlueShield, I’m referring to you! **
- Payment Rate: Payment from insurance companies changes based on client plan. The payment range is between $60-$98. Therapists who do not accept insurance typically charge $150+ per session.
- Frustration: Contacting the insurance company means going through an automated system, then dealing with a representative who “understands” the issues but can’t do anything to help except read from a script. Providers are unable to speak to a manager or receive a resolution in the moment; everything has to be “expedited” to an “adjuster” and then wait “7-10 business days” for a resolution. (Yes, I realize I’m putting everything in air quotes. The frustration is that it usually requires more than one round of “research” for BCBS to fix any issues.)
- Expensive: Therapists are only paid for the time they are face-to-face with a client; therefore, paperwork, claim submission, billing, etc. are unpaid work time. This means a provider must either: 1) use their time to contact the insurance company or 2) hire personnel to handle anything related to non-therapeutic tasks.
Deep Breath, Bree. Inhale… Exhale…
| Now that I have shared with all of you what the behind-the-scenes experience of dealing with insurance companies (specifically Anthem BCBS), I want to shift focus and share with you WHY I will continue to accept insurance for my clients:
|
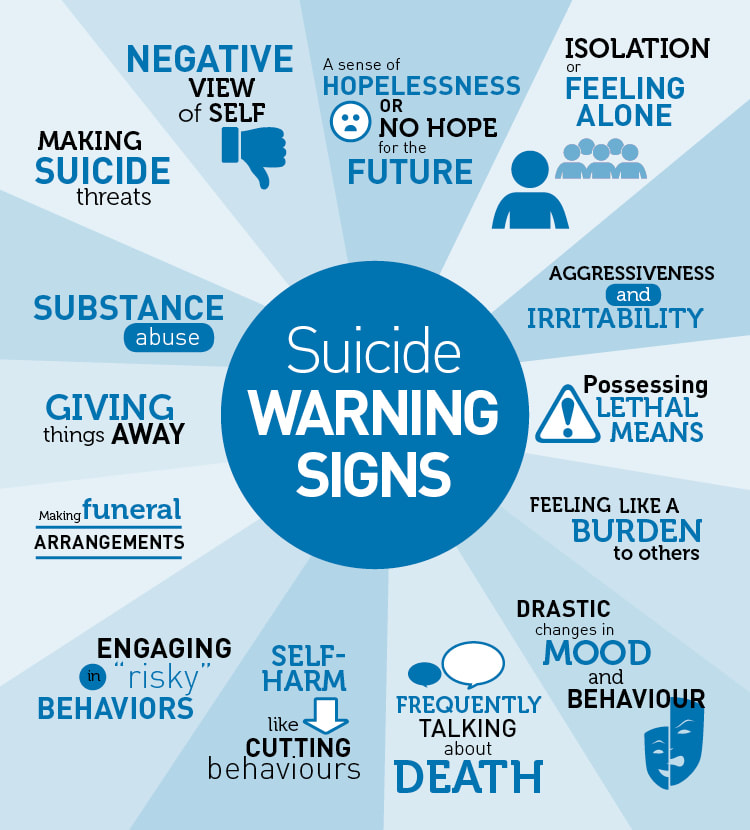
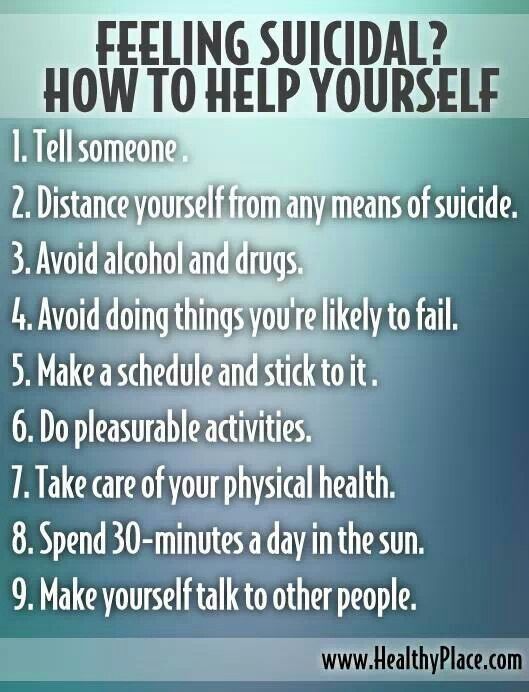
- Mental Health Awareness: Without effective mental health treatment, individuals living with depression and anxiety are in crisis. Access to therapy is need to prevent suicide and maladaptive living for individuals.
- Advocating: Insurance companies need to know that they are causing harm to individuals who are in dire need of mental health services. Denying access to services, underpayment of services, and/or lack of payment for services means some therapists will stop partnering with insurance companies.
It’s that simple (and complicated). People matter.
How can we get the insurance companies
(specifically Anthem BCBS) to realize this??
Author
Bree Winkler is a licensed professional counselor in Atlanta, GA. Bree helps clients manage anxiety, depression, anger, and relationship issues. She accepts Aetna and Anthem insurance plans, as well as private pay and offers receipts for out-of-network claims.





 RSS Feed
RSS Feed